Case Study : Application of Progressive Muscle Relaxation Methods in Third Trimester Pregnant to Reduce Fatigue During The Covid-19 Pandemic
Penerapan Metode Relaksasi Otot Progresif Pada Ibu Hamil Trimester Tiga Untuk Mengurangi Kelelahan Selama Pandemi Covid-19: Studi Kasus
Keywords:
Fatigue, progressive muscle relaxation (PMR), pandemic, third trimester pregnancyAbstract
Fatigue is the most common thing in third trimester pregnant women. Fatigue that occurs in third trimester pregnantwomen includes physiological and psychological aspects. Pregnancy during a pandemic is a new thing that challengingto pregnant women in social life. Pandemic also impact a social life of mother during the third trimester of pregnancy.The purpose of this paper is to analyze the implementation of nursing care in third trimester pregnant women whoexperience fatigue during a pandemic. Fatigue that occurs is often considered normal and a trigger factor for healthproblems of pregnant women and fetuses. One of an intervention to reduce fatigue in pregnant women is progressivemuscle relaxation. Progressive Muscle Relaxation (PMR) is a non-pharmacological action that focuses on relaxation ofthe mind and body that can reduce physiological and psychological fatigue in pregnant women. Provision of PMRintervention is given for 10 days. The results obtained were measured through pre and post intervention, there was adecrease in the level of fatigue by a mean difference of 4.3 (8.6%) as measured by the instrument MAF (MultidimentionalAssesment of Fatigue). Fatigue that previously disturbed activity to not interfere with daily activities. Based on that PMRintervention in third trimester pregnant women effectively reducing the level of fatigue so that pregnant women canmaintain their health status during a pandemic.Downloads
References
Akme?e, Z. B., & Oran, N. T. (2014). Effects of Progressive Muscle Relaxation Exercises Accompanied by Music on Low Back Pain and Quality of Life During Pregnancy. Journal of Midwifery and Women’s Health, 59(5), 503–509. https://doi.org/10.1111/jmwh.12176
Allen, D. G., Lamb, G. D., & Westerblad, H. (2018). Skeletal muscle fatigue: Cellular mechanisms. Physiological Reviews, 88(1), 287–332. https://doi.org/10.1152/physrev.00015.2007
American Pregnancy Association. (2020). Swelling During Pregnancy.
Anderson, S., & Bidner, C. (2018). Marriage, Commitment and Social Norms?: Theory and Evidence from Egypt ? - Preliminary and Incomplete -, 1–61.
Ashokka, B., Loh, M. H., Tan, C. H., Su, L. L., Young, B. E., Lye, D. C., … Choolani, M. (2020). Care of the pregnant woman with coronavirus disease 2019 in labor and delivery: anesthesia, emergency cesarean delivery, differential diagnosis in the acutely ill parturient, care of the newborn, and protection of the healthcare personnel. American Journal of Obstetrics and Gynecology. https://doi.org/10.1016/j.ajog.2020.04.005
Carington, A. (2020). Anxiety , depression increasing among mothers during the COVID-19 pandemic, 1–5. Retrieved from https://abcnews.go.com/Health/anxiety-depression-increasing-mothers-covid-19-pandemic/story?id=71605965
Charalambous, A., Giannakopoulou, M., Bozas, E., Marcou, Y., Kitsios, P., & Paikousis, L. (2016). Guided imagery and progressive muscle relaxation as a cluster of symptoms management intervention in patients receiving chemotherapy: A randomized control trial. PLoS ONE, 11(6), 1–18. https://doi.org/10.1371/journal.pone.0156911
Cheng, C. Y., & Pickler, R. H. (2014). Perinatal stress, fatigue, depressive symptoms, and immune modulation in late pregnancy and one month postpartum. The Scientific World Journal, 2014. https://doi.org/10.1155/2014/652630
Cronin, R. S., Chelimo, C., Mitchell, E. A., Okesene-Gafa, K., Thompson, J. M. D., Taylor, R. S., … McCowan, L. M. E. (2017). Survey of maternal sleep practices in late pregnancy in a multi-ethnic sample in South Auckland, New Zealand. BMC Pregnancy and Childbirth, 17(1), 1–7. https://doi.org/10.1186/s12884-017-1378-5
El-ati, I. H., & Amasha, H. A. (2015). Strategies Used by Women to Alleviate Heartburn during Pregnancy. Journal of Nursing and Health Science, 4(5), 1–8. https://doi.org/10.9790/1959-04510108
Forough, M., & Borzoee, F. (2017). Fatigue in Pregnancy. International Journal of Childbirth Education, 32(1), 10–12. https://doi.org/https://doi.org/10.18295/squmj.2019.19.01.009
Gök?in, ?., & Ayaz-Alkaya, S. (2018). The Effectiveness of Progressive Muscle Relaxation on the Postpartum Quality of Life: A Randomized Controlled Trial. Asian Nursing Research, 12(2), 86–90. https://doi.org/10.1016/j.anr.2018.03.003
Golmakani, N., Sadat, F., Ahmadi, S., Taghi, M., & Pour, N. A. (2015). Comparing the Effects of Progressive Muscle Relaxation and Guided Imagery on Sleep Quality in Primigravida Women Referring to Mashhad Health Care Centers -1393. Journal of Midwifery and Reproductive Health, 3(2), 335–342.
Hasanpour-Dehkordi, A., & Jalali, A. (2016). Effect of progressive muscle relaxation on the fatigue and quality of life among iranian aging persons. Acta Medica Iranica, 54(7), 430–436.
Ibanez, G., Khaled, A., Renard, J. F., Rohani, S., Nizard, J., Baiz, N., … Chastang, J. (2017). Back Pain during Pregnancy and Quality of Life of Pregnant Women. Primary Health Care Open Access, 07(01), 1–6. https://doi.org/10.4172/2167-1079.1000261
Kartilah, T., & Februanti, S. (2020). Effectiveness of progressive muscle relaxation and aromatherapy on fatigue in pregnant mothers. Medisains, 18(1), 14. https://doi.org/10.30595/medisains.v18i1.6421
Mallah, F., Tasbihi, P., Navali, N., & Azadi, A. (2014). Urinary incontinence during pregnancy and postpartum incidence, Severity and risk factors in alzahra and taleqani hospitals in Tabriz, Iran, 2011-2012. International Journal of Women’s Health and Reproduction Sciences, 2(3), 178–185. https://doi.org/10.15296/ijwhr.2014.26
Mortazavi, F., & Borzoee, F. (2019). Fear of Childbirth, Fatigue, and Well-being in Pregnant Women. Journal of Obstetrics, Gynecology and Cancer Research, 4(2), 45–50. https://doi.org/10.30699/jogcr.4.2.45
Pourjavad, M., & Mansoori, A. (2013). Study of Fatigue in Working Pregnant Women, 17(1), 35–40.
Qian, X., Ren, R., Wang, Y., Guo, Y., Fang, J., Wu, Z. D., … Han, T. R. (2020). Fighting against the common enemy of COVID-19: A practice of building a community with a shared future for mankind. Infectious Diseases of Poverty, 9(1), 4–9. https://doi.org/10.1186/s40249-020-00650-1
Ricci, S.S. (2017). Essentials of Maternity, Newborn, and Women's Health Nursing. Philadelphia : Wolters Kluwers Lippincott William & Willkins
Sadeghi, A., Sirati-Nir, M., Ebadi, A., Aliasgari, M., & Hajiamini, Z. (2015). The effect of progressive muscle relaxation on pregnant women’s general health. Iranian Journal of Nursing and Midwifery Research, 20(6), 655. https://doi.org/10.4103/1735-9066.170005
Sangsawang, B., & Sangsawang, N. (2013). Stress urinary incontinence in pregnant women: A review of prevalence, pathophysiology, and treatment. International Urogynecology Journal, 24(6), 901–912. https://doi.org/10.1007/s00192-013-2061-7
SDKI DPP PPNI. (2017). Standar Diagnosis Keperawatan Indonesia (1st ed.). DPP PPNI.
SIKI DPP PPNI. (2018). Standar Intervensi Keperawatan Indonesia (1st ed.). DPP PPNI.
Simarmata, I., Budihastuti, U., & Tamtomo, D. (2019). Effect of Social Suport and Social Interaction on Anxiety Among Pregnant Women. Journal of Maternal and Child Health, 4(4), 287–293. https://doi.org/10.26911/thejmch.2019.04.04.08
Taghizadeh, Z., Irajpour, A., & Arbabi, M. (2013). Mothers’ response to psychological birth trauma: A qualitative study. Iranian Red Crescent Medical Journal, 15(10), 1–7. https://doi.org/10.5812/ircmj.10572
van de Loo, K. F. E., Vlenterie, R., Nikkels, S. J., Merkus, P. J. F. M., Roukema, J., Verhaak, C. M., … van Gelder, M. M. H. J. (2018). Depression and anxiety during pregnancy: The influence of maternal characteristics. Birth, 45(4), 478–489. https://doi.org/10.1111/birt.12343
World Health Organization. (2020). Gender and COVID-19. WHO : Genewa.
Zahoor, S., Babar, M. E., Javed, M. M., & Hussain, T. (2018). Constipation in pregnancy: Causes and remedies. Progress in Nutrition, 20, 305–311. https://doi.org/10.23751/pn.v20i1-S.5788
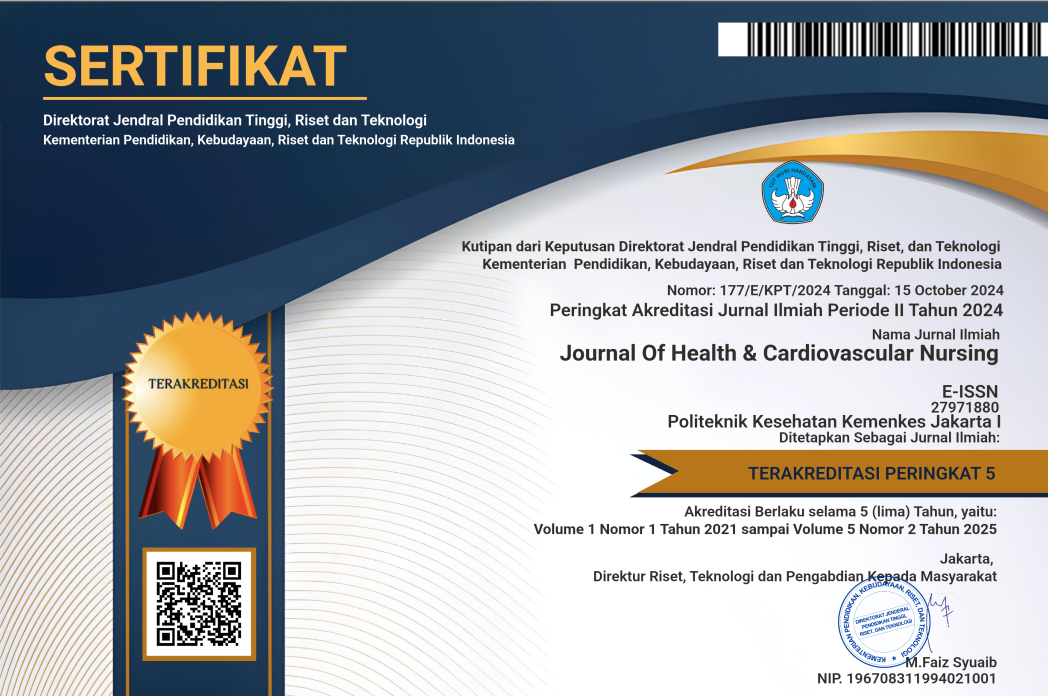
Published
Issue
Section
Copyright (c) 2023 Journal of Health and Cardiovascular Nursing

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.